Atheroembolism is a complication of cardiac catherization
- Risk of cardiac catherization is small. One risk is atheroembolism
- Atheroembolism: atherosclerotic fragments dislodged from aortic wall and embolizes elsewhere
- Sx:
- livedo reticularis or blue toe syndrome
- Other locations: kidney (renal failure), retina, cerebrum, GI
Case:
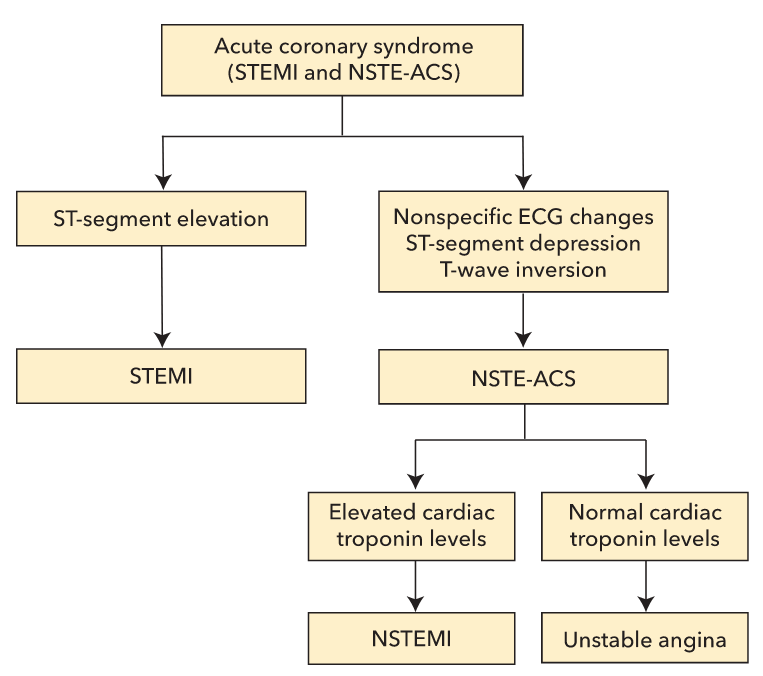
A 68-year-old male with a past medical history of hypertension, hyperlipidemia, type 2 diabetes mellitus, and transient ischemic attacks is admitted to the hospital for chest pain. He complains of episodic substernal chest pain that radiates down his left arm for approximately 25-30 minutes. The pain is not related to exertion. He denies having palpitations, shortness of breath, nausea, vomiting, or sweating. He had a carotid endarterectomy five years ago. He has smoked one-half pack of cigarettes per day for the last 30 years and drinks alcohol occasionally. He has a strong family history of hypertension, stroke, and myocardial infarction. After his initial evaluation, an ECG is obtained that shows non-specific ST segment abnormalities in the inferior and lateral leads. The cardiac troponin T level is negative. A cardiac catheterization is performed, showing 50% atherosclerotic stenosis of the proximal left anterior descending artery and 70% atherosclerotic stenosis of the distal right coronary artery. No intervention is undertaken. On the third day of hospitalization, the patient continues to complain of occasional chest pain. His BUN level is 42 mg/dL and his serum creatinine level is 1.9 mg/dL (in comparison to a BUN of 19 mg/dL and a creatinine of 0.9 mg/dL on the day of admission). Physical examination now shows a purple discoloration of his right third toe. Which of the following additional laboratory findings would you most expect in this patient?